There are 6 steps of the procedure, which generally takes 2 to 3 hours.
Step 1: prepare the patient
You will lie on the operating table and be given general anesthesia. Once you are asleep, your nose is prepped with antibiotic and antiseptic solution.
An image-guidance system may be placed on your head (Fig. 2). This device is like a global positioning system (GPS) and helps the surgeon navigate through the nose using a 3D “map” created from your CT or MRI scans.
Step 2: make an incision
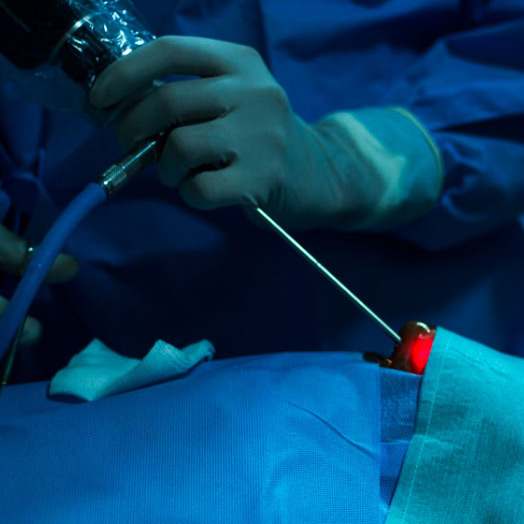
The ENT surgeon inserts the endoscope in one nostril and advances it to the back of the nasal cavity. An endoscope is a thin, tube-like instrument with a light and a camera. Video from the camera is viewed on a monitor. The surgeon passes long instruments through the nostril while watching the monitor. A small portion of the nasal septum dividing the left and right nostril is removed. Using bone-biting instruments, the front wall of the sphenoid sinus is opened
Step 3: open the sella
At the back wall of the sphenoid sinus is the bone overlying the pituitary gland, called the sella. The thin bone of the sella is removed to expose the tough lining of the skull called the dura. The dura is opened to expose the tumor and pituitary gland.
Step 4: remove the tumor
Through a small hole in the sella, the tumor is removed by the neurosurgeon in pieces with long grasping instruments
The center of the tumor is cored out, allowing the tumor margins to fall inward so the surgeon can reach it. After all visible tumor is removed, the surgeon advances the endoscope into the sella to look and inspect for hidden tumor. Some tumors grow sideways into the cavernous sinus, a collection of veins. It may be difficult to completely remove this portion of the tumor without causing injury to the nerves and vessels. Any tumor left behind may be treated later with radiation.
At some hospitals, surgery can be performed in a special OR room equipped with an intraoperative MRI scanner. The patient can undergo an MRI during surgery. This gives the surgeon real-time images of the patient’s brain to know exactly how much tumor has been removed before ending the procedure. This technology enables more complete tumor removal and may reduce the need for a second operation [1].
Step 5: obtain fat graft (optional)
After tumor is removed, the surgeon prepares to close the sella opening. If needed, a small (2cm) skin incision is made in the abdomen to obtain a small piece of fat. The fat graft is used to fill the empty space left by the tumor removal. The abdominal incision is closed with sutures.
Step 6: close the sella opening
The hole in the sella floor is replaced with bone graft from the septum (Fig. 5). Synthetic graft material is sometimes used when there is no suitable piece of septum or the patient has had previous surgery. Biologic glue is applied over the graft in the sphenoid sinus. This glue allows healing and prevents leaking of cerebrospinal fluid (CSF) from the brain into the sinus and nasal cavity.